Va Medical Claims For Providers
If you're looking for video and picture information related to the keyword you have come to visit the right site. Our site provides you with hints for viewing the highest quality video and image content, search and locate more informative video content and images that fit your interests.
comprises one of thousands of video collections from various sources, particularly Youtube, therefore we recommend this video for you to see. It is also possible to contribute to supporting this website by sharing videos and graphics that you enjoy on this blog on your social networking accounts such as Facebook and Instagram or educate your closest friends share your experiences concerning the simplicity of access to downloads and the information you get on this website. This blog is for them to visit this website.
Private Provider Information The Veterans Benefits Administration VBA uses VA Form 21-4142 Authorization to Disclose Information to the Department of Veterans Affairs VA to request private medical records and information regarding the source of records in support of claims for compensation andor pension benefits.
Va medical claims for providers. To access Availitys Claim Research Tool. If you applied online with VONAPP Direct Connect you should see receipt in your list of Open Claims within one hour. Apply for VA health care find out how to access services and manage your health and benefits online. Do not submit medical documentation to WPS MVH along with claims.
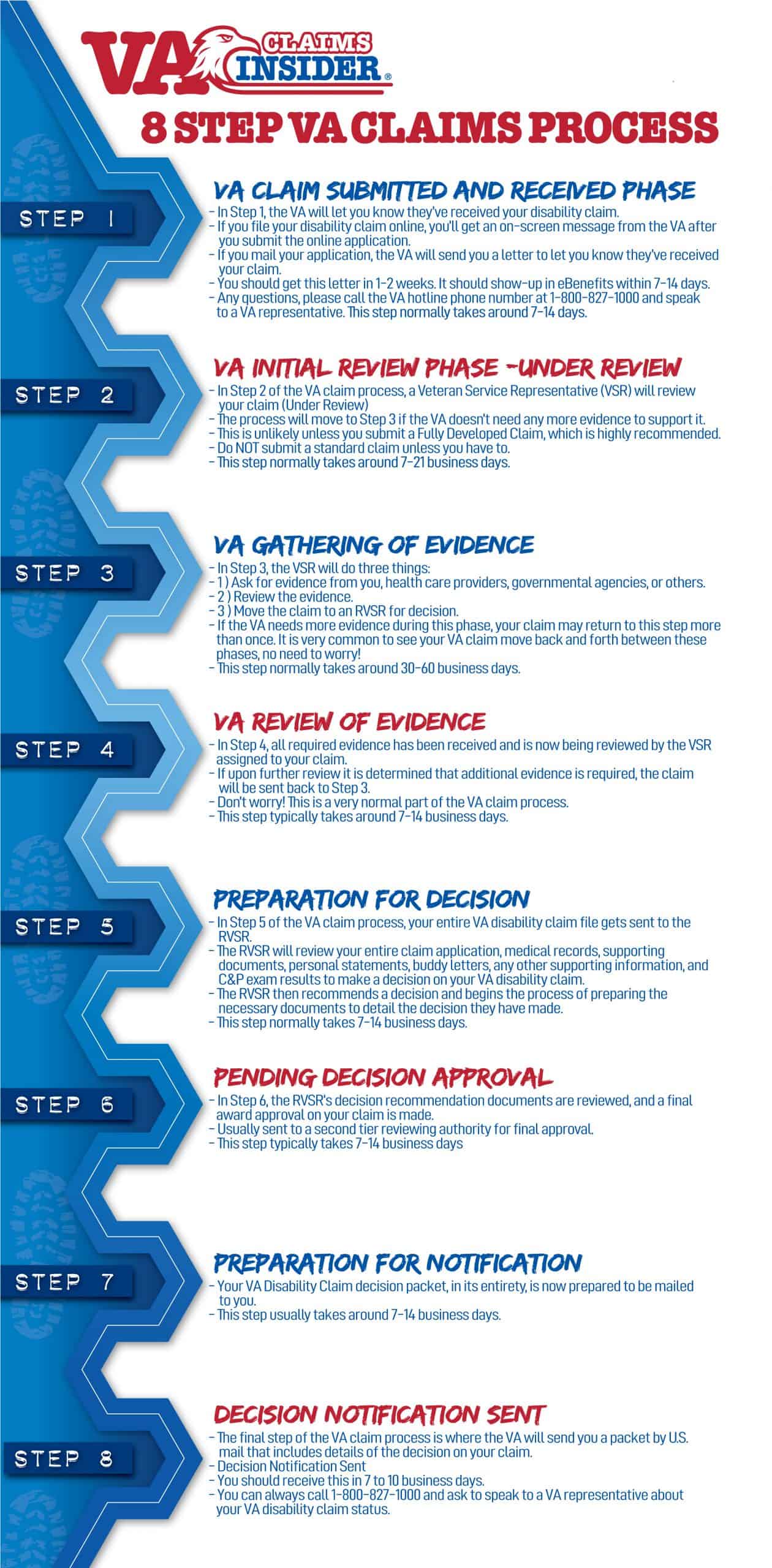
The eight steps of claims processing are as follows. Claims Submission on Paper Paper claims should be submitted by mail to. A Medical Opinion MO comes from the examining physician at your CP exam whereas an Independent Medical Opinion IMO also known as a Medical Nexus Letter can come from any private medical provider and is used to help a veteran prove VA service connection. Once you file a claim for care provided to a Veteran or Veteran family member VA adjudicates the claim and provides an electronic payment.
2 If VACC andor Provider Agreements you would be receiving authorizations and sending claims directly to your local VA medical center VAMC. Providers can check Veterans Choice Program VCP and Patient-Centered Community Care PCCC claims status online using the Availity Claim Status Tool. The process for submitting claims as an ancillary provider applies to both participating and nonparticipating providers. ECAMS is expected to be implemented nationwide between March and August 2019.
The system modernizes the processing of claims received by community providers outside VAs Community Care Network CCN. You are strongly encouraged to submit as much evidence as possible with your claim to help minimize processing time. Disability File a claim for disability compensation for conditions related to your military service and manage your benefits over time. From that point forward community providers are to send medical records to the referring VA Medical Center VAMC.
Thanks to the recently approved Johnny Isakson and David P. Box 30780 Tampa FL 33630-3780. While not required to process a claim for authorized services medical documentation must be submitted to the authorizing VA medical facility as soon as possible after care has been provided. Electronic Claims Adjudication Management System eCAMS eCAMS is a community care claims processing software solution being implemented by VA.
WPS MVH-VAPCCC PO Box 7926 Madison WI 53707-7926. There are multiple methods by which community providers may electronically provide VA with the required medical documentation for care coordination purposes. Your claim has been received by the VA. Please note that community health care providers must have their own Direct Messaging system to send and receive Veteran health information via VA Direct Messaging.
Veterans Health Care and Benefits Improvement Act of 2020 publication and acceptance of VA DBQ forms are now codified in federal law. Community providers who submit paper claims and supporting documentation should submit those documents to. The passage of this new Bill protects veterans and private healthcare providers who wish to use a private DBQ as medical evidence to support their VA disability compensation claims. This tool is a fast easy-to-use online claim status tool that provides real-time claim status and payment information.
Return to VHIE Home. For more information view the Medical Documentation Update on the HNFS website or call the HNFS Provider Service Line. VA is required to pay all medical and dental claims from providers electronically. If you as a community health care provider need technical support regarding VA Direct Messaging please contact VADirectSupportvagov.
If you are a community provider interested in providing care to Veterans please consider joining the new VA Community Care Network. For claims submitted to one of VAs Third Party Administrators TPAs such as TriWest Healthcare Alliance for care provided through the Veterans Choice Program VCP or Patient-Centered Community Care PC3 networks you will receive a payment from the same TPA. VA is transitioning paper claims and supporting documents for community care to an electronic format in order to improve the claims submission and processing capabilities. HNFS Provider Service Line.
Community providers are a vital part of VAs high-performing health care network ensuring eligible Veterans and their beneficiaries get the timely high-quality health care they need.