Va Disability Sleep Apnea Secondary To Anxiety
If you're looking for picture and video information linked to the key word you've come to visit the right site. Our website provides you with suggestions for viewing the maximum quality video and image content, hunt and locate more enlightening video content and images that fit your interests.
comprises one of tens of thousands of movie collections from several sources, especially Youtube, therefore we recommend this video that you see. This blog is for them to visit this website.

Sleep Apnea with Obesity as an Interim Link.
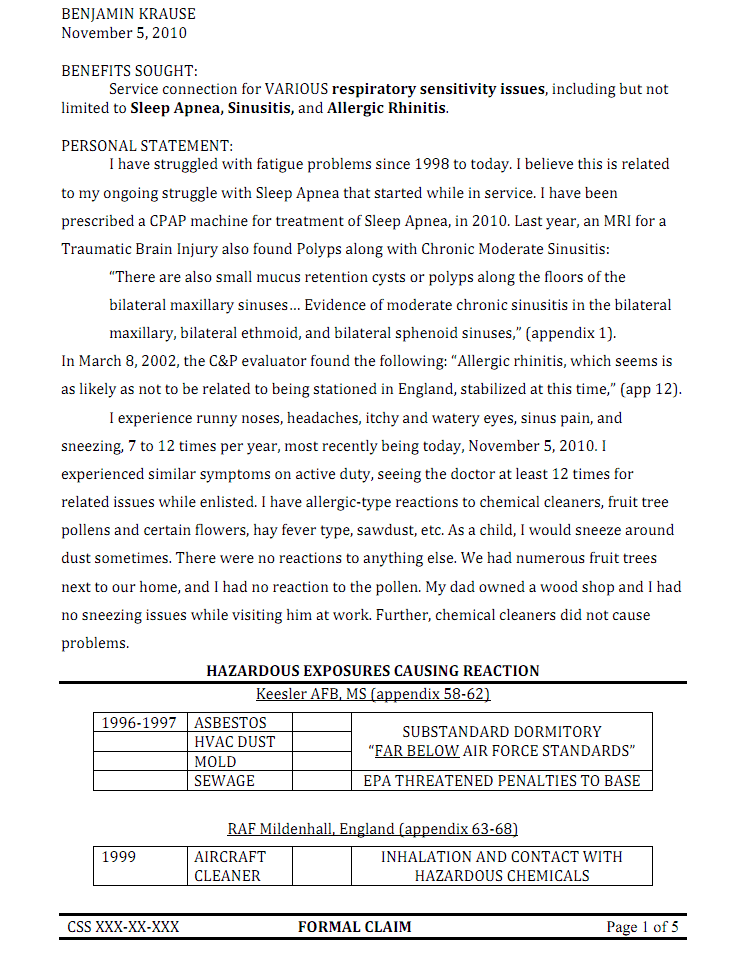
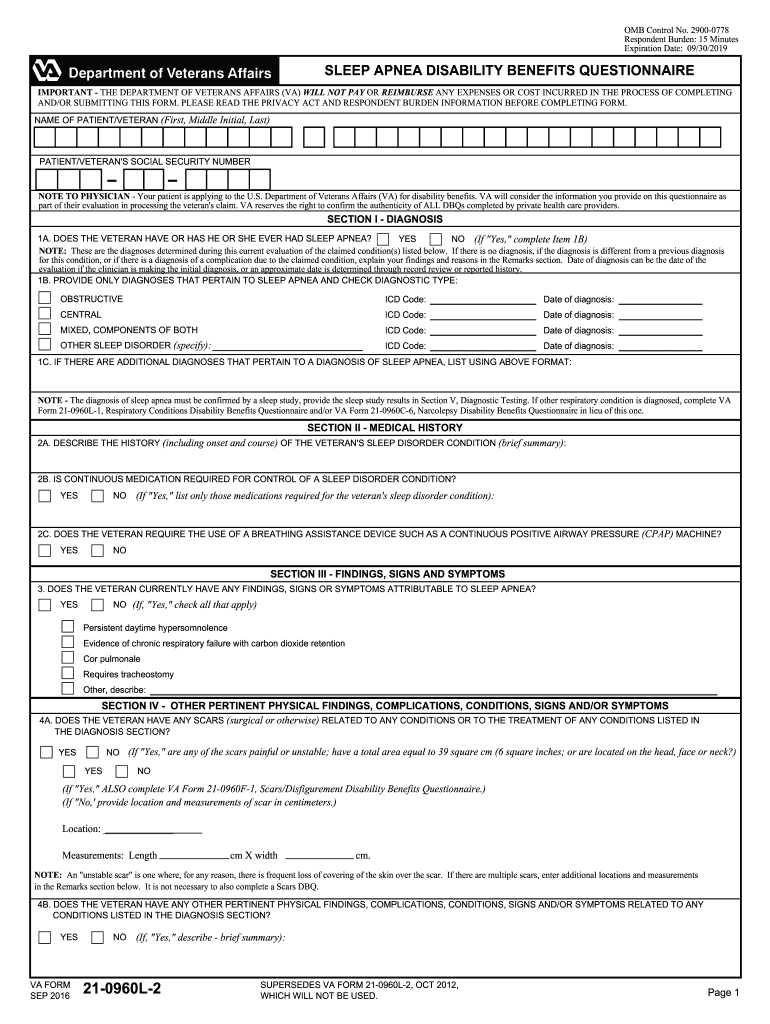
Va disability sleep apnea secondary to anxiety. A medical diagnosis of sleep apnea confirmed by a sleep study in VA medical records or private records sleep study in past 12 months Evidence of a service-connected primary disability such as PTSD depression anxiety sinusitis rhinitis weight gain AND. Studies show us that while 4 of American men suffer from sleep apnea the percentage of OSA sufferers with depression 22 anxiety disorders 17 and PTSD 11 is much higher than in the general population. Specifically people who suffer from sleep apnea are 21-39 percent more likely to have depression than those who do not have sleep apnea. When a Veteran starts considering whether or not to file a VA Disability Claim there are a lot of questions that he or she tends to ask.
VA offers service-connected compensation for multiple sleep disturbances including sleep apnea insomnia and narcolepsy. That stress makes hormones which increase blood pressure levels. VA Disability Claims General Sleep Apnea Secondary to AnxietyObesity. Importantly service connection for sleep disorders can be awarded on a direct secondary or presumptive basis.
I have been successfully Service Connected for Obstructive Sleep Apnea 50 Secondary to Anxiety. Many veterans struggle with mental illnesses like depression and PTSD and many veterans suffer from sleep apnea. If you have a doctor that does that then you can link the sleep apnea as being causedaggravated by the anxietywhatever sc disability. Anxiety and depression can make sleep apnea worse but there is no solid evidence that they cause sleep apnea.
Among the risk factors for OSA Obesity is perhaps the most important and the most commonly accepted connection to Sleep Apnea disorders. These types of sleep disturbances may be secondary to other service-connected conditions like PTSD. Many veterans obtain spinal problems from their time in the service from accidents. Because of this it will be difficult if not impossible to claim sleep apnea as secondary to anxiety and depression.
A medical diagnosis of sleep apnea confirmed by a sleep study in VA medical records or private records unless you did this already on active duty Evidence of a service-connected primary disability such as PTSD depression anxiety sinusitis rhinitis weight gain AND. There is a well-known correlation between mental illnesses and obstructive sleep apnea OSA. The VA also offers benefits for sleep disorders like obstructive sleep apnea and hypersomnolence which can include narcolepsy and insufficient sleep syndrome. I just won my claim for depression and anxiety secondary to sleep apnea.
Patients with sleep apnea suffer a lack of oxygen which may cause changes to the brain resulting in depression. Chronic Tinnitus taps the brains precuneus region more during episodes. Several cross-sectional studies have consistently found an association between increased body weight and the risk of developing Sleep Apnea. Over the last 10 years the following are the 14 most common basic.
Some of the most common secondary service-connected disabilities from sleep apnea are high blood pressure heart disease type 2 diabetes weight gain asthma and even acid reflux disease. If you are able to service-connect your sleep apnea you may also receive hypertension VA disability benefits. There are multiple theories suggesting why this correlation may exist including the following. If you can get a Nexus letter from a physician however it may still be worth submitting a claim.
Clinical journal concluded that patients with chronic Tinnitus had increased brain attention.