Va Claims Process For Providers
If you're searching for video and picture information linked to the key word you have come to pay a visit to the right blog. Our site gives you hints for viewing the highest quality video and picture content, search and locate more enlightening video content and graphics that match your interests.
comprises one of thousands of video collections from various sources, especially Youtube, so we recommend this video that you view. This site is for them to stop by this website.

File your claim by mail using an Application for Disability Compensation and Related Compensation Benefits VA Form 21-526EZ.
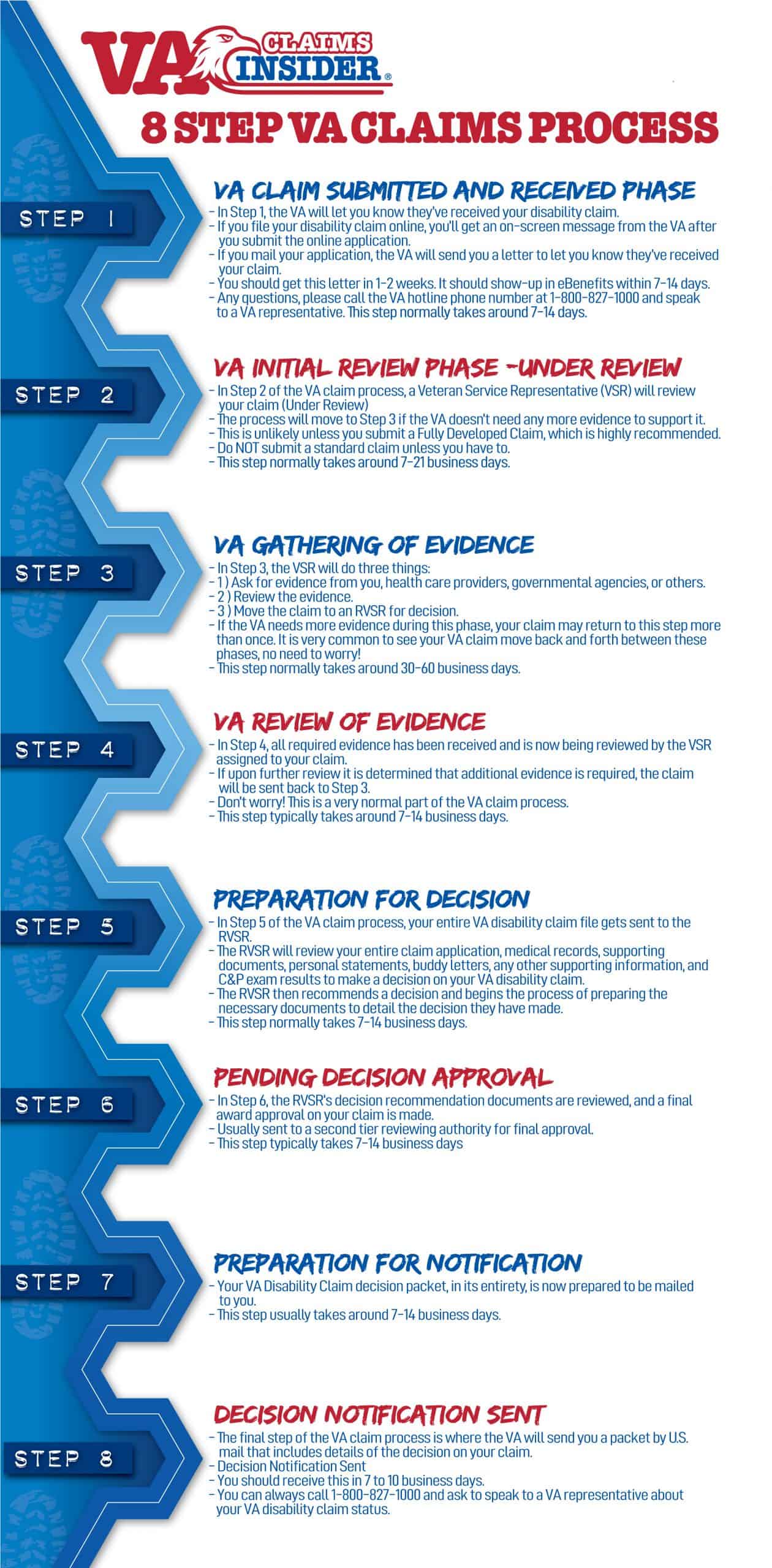
Va claims process for providers. You should get this letter about one week plus mailing time after we receive your claim. There youll see a summary of the latest status information for any open claims or appeals you may have. The provider participates in the VAs contracted network Patient-Centered Community Care PC3 administered by TriWest Healthcare Alliance a Third Party Administrator TPA under contract with VA AND. This step is the longest phase in the VA claim process and usually takes 30-60.
VA is transitioning paper claims and supporting documents for community care to an electronic format in order to improve the claims submission and processing capabilities. If you mail your application well send you a letter to let you know we have your claim. Go to your My VA dashboard. Click on the View Status button for a specific claim.
A request for reconsideration is a request from a claimant for the Department of Veterans Affairs VA to reconsider one of its decisions that has not yet become final the one-year appeal period which begins on the date the claimant was notified of the decision at issue has not yet expired. Submission Process for Veteran Community Care Claims and Supporting Documents. Private Provider Information The Veterans Benefits Administration VBA uses VA Form 21-4142 Authorization to Disclose Information to the Department of Veterans Affairs VA to request private medical records and information regarding the source of records in support of claims for compensation andor pension benefits. If you file your claim online youll get an on-screen message from us after you submit the form.
Youll find the link for this dashboard in the top right corner of the page once youre signed in. Download VA Form 21-526EZ PDF Print the form fill it out and send it to this address. Submit VA Form 21-0966 Intent to File a Claim for Compensation andor Pension or Survivors Pension andor DIC You can access this form at. Your claim has been received by the VA.
This step typically takes 7 to 21 days STEP 3. If you applied online with VONAPP Direct Connect you should see receipt in your list of Open Claims within one hour. Providers may submit electronic claims via any software clearinghouse or billing service which is a WPS Health Solutions approved Trading Partner for electronic claims submission. If you are a community provider interested in providing care to Veterans please consider joining the new VA Community Care Network.
ECAMS is expected to be implemented nationwide between March and August 2019. Community providers who submit paper claims and supporting documentation should submit those documents to. Normally takes between 7 and 14 days STEP 2. Department of Veterans Affairs Claims Intake Center PO Box 4444 Janesville WI 53547-4444.
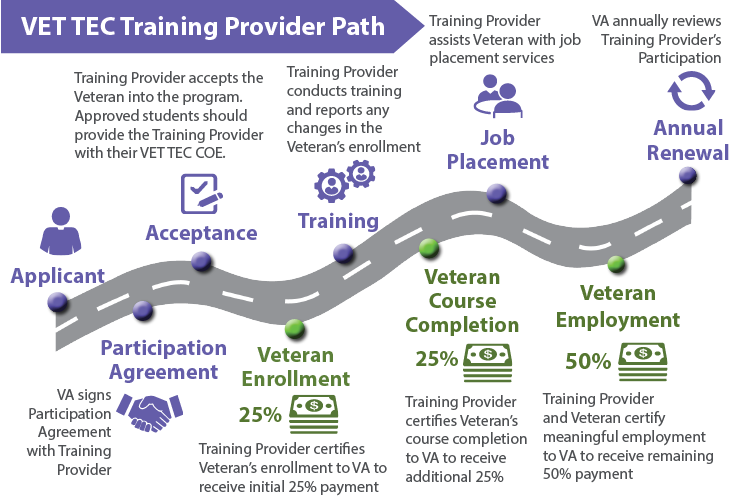
Community providers are a vital part of VAs high-performing health care network ensuring eligible Veterans and their beneficiaries get the timely high-quality health care they need. As part of its efforts to improve services for Veterans VA developed this video Community Care Claims Process that explains the community care claims submission process and provides suggestions on ways to help community providers receive prompt payment for the services they provide to Veterans. 2 If VACC andor Provider Agreements you would be receiving authorizations and sending claims directly to your local VA medical center VAMC. If you need more time to collect support for your claim you may use the optional intent to file process.
Community providers caring for Veterans through VCP may continue to provide Veteran care if both the following criteria are met. The system modernizes the processing of claims received by community providers outside VAs Community Care Network CCN. If you applied through the US. Mail please allow mailing time plus one week for us to process and record receipt of your claim.
If you file your claim on eBenefits youll see a notice from us in your claims list within about one hour of applying. VA Disability Claim Process Timelines After Claim Submission STEP 1. Scroll down to the Track Claims section. Box 30780 Tampa FL 33630-3780.